Persistence of Lyme patients and the role of patient organizations
Patients respond to chronic under-diagnosis and treatment of Lyme disease in Canada.

What happens when growing numbers of patients are unable to receive a diagnosis and adequate treatment for Lyme disease? They keep looking for solutions, both individually and collectively. This in-depth article by Cox and Levesque gives context to many of the systemic barriers that Canadian Lyme patients encounter, and highlights the important role that patient organizations play in addressing those barriers.1
The divergence between the lived patient experience and clinical evidence defended by influential scientists threatens the health and well-being of patients whose symptomology does not conform to guidelines sanctioned by health authorities.
Marilyn Cox and Mario Levesque
The authors discuss the interface between various scientific approaches and the reality and experience of patients in the context of limited clinical and scientific evidence. They point out that selected experts can become gatekeepers for research, health policy and for direct access to healthcare. They cite guidance from The Nova Scotia Infectious Diseases Expert Group that includes strict diagnostic criteria, preventing many patients from receiving diagnosis and treatment.
Cox and Levesque also review the historical role that patient organizations have played in supporting patients and the challenges these organizations encounter when lobbying for changes to healthcare policy. They note that Lyme disease (LD) organizations are established in response to the disparity between patient experiences and medical authority, and present an approach that values scientific evidence, clinical judgement and expertise.
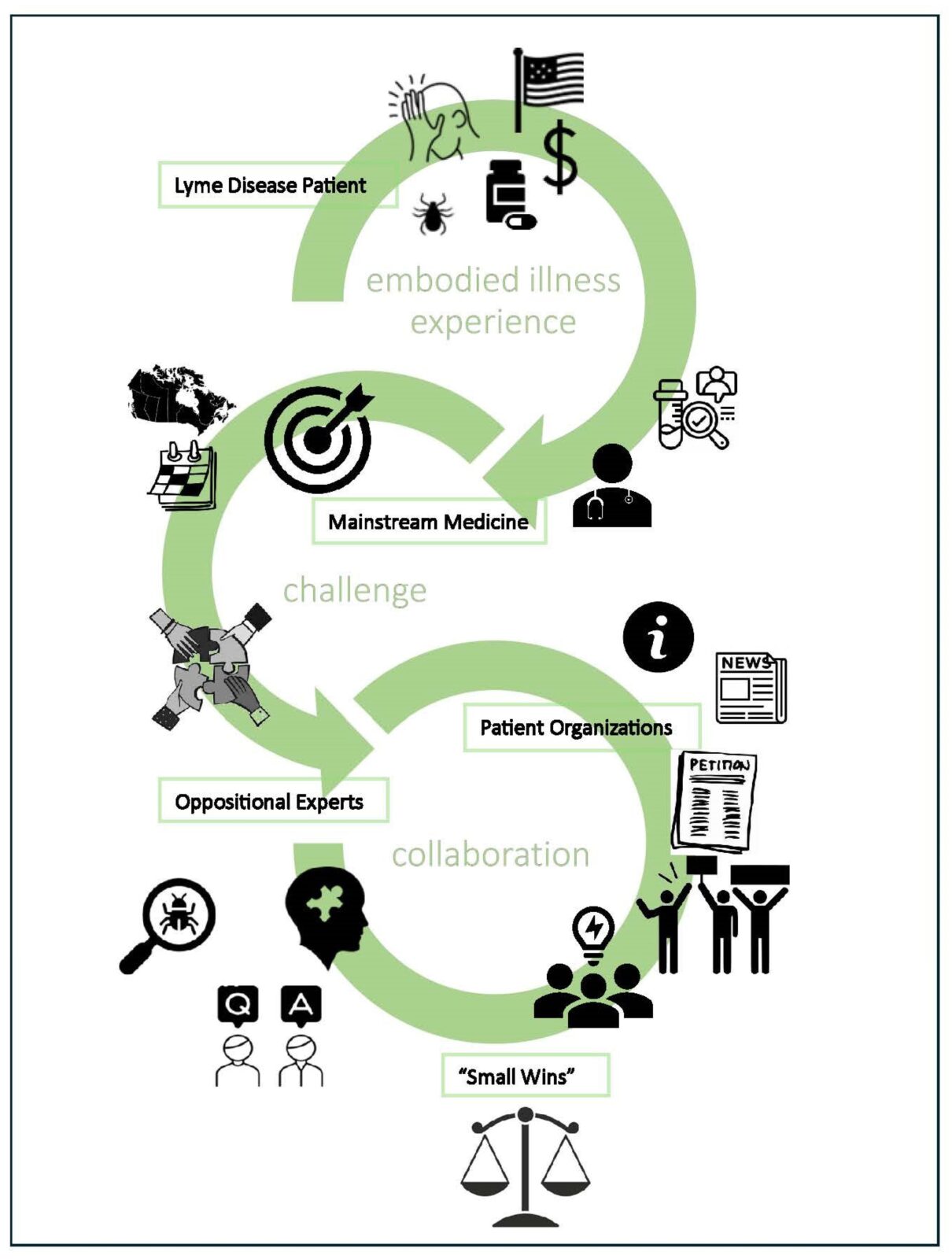
Using the framework of embodied health movements, we highlight the motivation and mobilization of LD patient organizations and a need for the mutual appreciation of scientific evidence, clinical judgement, and experiential knowledge.
The emphasis is on evidence-informed medicine as a tenet of person-centred medicine with the understanding that scientific knowledge is a means to support rather than limit clinical judgement.
The authors clearly articulate what lies at the core of the problem; a restrictive and outdated understanding of Lyme disease that is sustained by the approach and guidelines set out by the Infectious Diseases Society of America (IDSA), and is supported by health authorities and associations in Canada. This understanding fails to take into account the scientific and clinical evidence regarding persistence of the bacteria, the effect of the bacteria on the immune system and inflammation, interactions with other infections in the body and the chronic and complex manifestations of the disease.
Physicians are pressured to conform to guidelines that limit clinical judgement and do not adequately address LD cases.
Patients and patient organizations also have a critical role to play in ongoing research. Cox and Levesque discuss the events that followed the 2016 Conference to develop a framework on Lyme disease, a conference that was designed to develop a better understanding of Lyme disease.
Over five hundred patients, caregivers, health professionals, representatives from the federal government, PHAC, CanLyme, and AMMI were in attendance. Many LD patients spoke at the conference, sharing personal experiences with misdiagnosis, a lack of awareness of LD, the failure to provide treatment options, and inaccurate testing and reporting. CanLyme president Jim Wilson stressed the need for patients to be equal partners in LD health policy.
Both the framework and the allocation of research funding that followed failed to reflect and appreciate the importance of the patient voice in terms of policy and research.
Despite assurances given by health officials and politicians at the 2016 conference, patient organizations were denied a role with funds given entirely to the newly formed Canadian Lyme Disease Research Network (CLyDRN).
One must be wary of ambiguous terms like “patient engagement” that allow token participation but deny authority. The objective is an equal partnership with other stakeholders for transparency and accountability and to ensure that the lived experience of LD is fairly represented and heeded.
The authors review many of the initiatives that patients and patient organizations have embarked upon over the years, and point to future hope with patient driven funding and the persistence of patient organizations in working toward patient-centered solutions.
Citation
Cox M, Levesque M. “Small Wins” for those with Lyme Disease in Canada: Patients in an Embodied Health Movement. Zoonotic Diseases. 2024; 4(1):22-36. https://doi.org/10.3390/zoonoticdis4010004
Graphical abstract